CHR’s Preliminary 2025 IVF Cycle Outcomes
Today’s posting presents preliminary IVF cycle outcome data of the CHR for the year 2025. It is important to emphasize the preliminary nature of these data because they – due to the timing of this analysis - of course cannot yet include live birth rates.
Here reported ongoing clinical pregnancy rates, therefore, do not yet include all miscarriages (very early miscarriages - so-called chemical pregnancies - of course, have already been excluded). Considering the unusually advanced female age of the CHR’s patient population and the unusually high prevalence of other adverse outcome parameters (like number of previously failed IVF cycles, numbers of prior IVF clinics utilized, abnormally low FSH & AMH values, etc.), miscarriage rates can be expected to be significantly higher than in average national data sets.
It is also important to reemphasize that outcome percentages are reported as percentage of ongoing clinical pregnancies with reference point embryo transfer in women who had at least one cleavage stage (day-3 after fertilization) embryo for transfer. This is, indeed, a relatively low qualification threshold because it does not require that an embryo reaches blastocyst stage (which would bias patient selection toward patients with better prognosis).
The reason for this reference point is once again the very adversely selected patient population the CHR is serving, where over half of all patients – before reaching the CHR – were advised that they no longer could conceive with use of their own eggs and basically had no other choice but third-party egg donation. As one would expect, in such a patient population, being unable to produce even a single day-3 embryo will not be uncommon, a fact also in detail explained in the informed consent process the CHR’s unfavorable prognosis patients undergo before being started in an IVF cycle.
Like most IVF clinics, the CHR (and all other IVF clinics) – usually around November – report final annual outcome data for the preceding year (at a time when live birth rates can be known already) to the CDC as well as ASRM/SART registries, - where they become publicly available.
And then something - by now already pretty funny – usually happens: Especially the ASRM/SART registry, after reviewing submissions - laudably – often checks on the accuracy of submitted data that fall outside of national statistical probabilities. And, since the CHR’s patient population does that in so many different ways and statistical parameters, it usually means that the CHR staff ends up answering many such inquiries. And last year, indeed, ASRM/SART even sent out an auditor to confirm the center’s data submission.
All of this is, of course, a tortious process that takes time, which is the reason why the CDC and ASRM/SART registries report final data with 2- to 3-year delays. They are, however, by far the best IVF outcome data published by any registry in the world and are steadily further improved, thereby becoming an increasingly important resource for interesting and important IVF research. With the A.I. revolution in full swing, we are expecting continues additional progress at greatly increased speed and, hopefully, shorter delays in publications of these annual reports.
The CHR’s Editorial Staff
CHR’s Preliminary 2025 IVF Cycle Outcomes
Patient Population
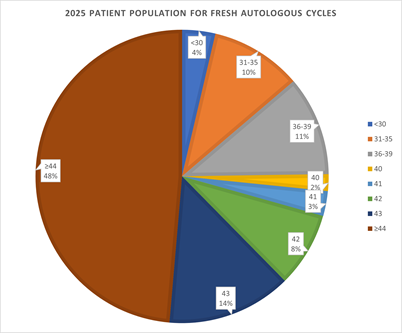
As the pie chart below demonstrates, the CHR’s patient population in 2025 undergoing autologous IVF cycles (IVF cycles with use of their own eggs) was once again by far the oldest among U.S. IVF clinics (and likely in the world. The median age was “only” 44, - meaning that the CHR’s patients in 2025 became a year younger than in 2024. But, still, 48% of patients were over age 44 (going up into the 50s). Remarkably, only 25% of patient were under age 40 and almost all of these “younger” patients demonstrated low functional ovarian reserve (i.e., suffered from premature ovarian aging, POA)
And the boxes below demonstrate cycle outcomes if a patient had at least one day-3 (cleavage-stage) embryo available.
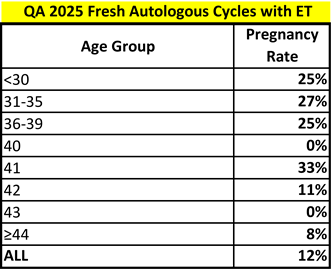
Clinical Pregnancy Rates
FRESH AUTOLOGOUS CYCLES -- The first box demonstrates autologous ongoing clinical pregnancy rates in different age groups, - as the box demonstrates, cumulatively the CHR’s clinical pregnancy rate in this very unfavorable patient population remained steady at 12%, exactly where it was in 2024. In practical terms this means that we were not able in 2025 to continue the year-to-year improvement in cycle outcomes we witnessed between 2022 and 2024, where we improved from 8% to 10%, and then in 2024 to an overall ongoing clinical pregnancy rate of 12%.
This should not surprise because in 2025 – in contrast to the three preceding years - the CHR did not introduce any major new practice patterns, as we had between 2022 and 2024 with the introduction of Highly Individualized Egg Retrieval (HIER) and progressively earlier egg retrievals at smaller and smaller lead follicle sizes. By again demonstrating the same 12% ongoing clinical pregnancy rate as in the preceding year, 2025, however, reaffirmed that 12% clinical pregnancy rate per cycle IVF cycle start is what the CHR’s highly unfavorable patient population now, however, can solidly expect if they manage to produce as little as only 1 day-3 embryo. And this is a remarkable result, considering patients reaching the CHR routinely report that they were quoted pregnancy chances of 1-2%,
A final word of caution is here, however still in place: As here reported cycle outcomes are only ongoing clinical pregnancy rates (final live birth rates for 2025 will not be available till October), we, of course, expect a significant miscarriage rate in a population of so advanced age and with such poor functional ovarian reserve (FOR) as the CHR serves.
The 0 rates at ages 40 and 43 are reflections of very small cycle numbers at these age groups. Likely the most remarkable age group in this date were the women above age 44 (which included women into the early 50s) who demonstrated an 8% ongoing pregnancy rate. Truly remarkable and strong evidence that - with further study and a further improving understanding of older women’s ovarian physiology – even further progress can probably be achieved even at these extremely advanced ages.
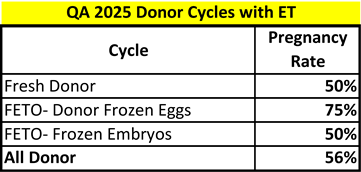
DONOR EGG CYCLES – Because donor-egg cycles in a large majority involve young and carefully selected egg donors, they produce the by-far highest clinical pregnancy rates and lowest clinical miscarriage rates. Moreover, under quite strict regulatory guidelines donor selection is quite uniform. Fresh donor egg cycles, therefore, have historically been considered the most objective reflection of an IVF clinic’s embryology laboratory quality, - as most important confounders for cycle outcomes, like age and FOR, fall by the wayside because nobody selects older women with low FOR as donors.
And – as demonstrated in the box below - the CHR’s clinical pregnancy rates in donor cycles, whether with fresh or frozen donor eggs or whether with partner or donor semen (donor embryo) were, indeed, truly remarkable (see box below). Once again, these numbers must be interpreted in consideration of the CHR’s patient population which is not only much older than patients at all U.S. (and likely worldwide) IVF clinics, but also have failed more IVF cycles, including prior donor egg cycle.
Here presented numbers include all cycles in which at least 1 day-3 or day-5/6/7 embryo was transferred. Once again, we, however, want to point out that these are ongoing pregnancy and not yet live birth rates and that miscarriage rates at this stage cannot yet be determined. Considering the young age of egg donors, miscarriage rates in this group of cycles can, however, be expected to be very small in comparison to above noted autologous oocyte cycles.
FETO denotes us of frozen donor eggs or frozen embryos using donor eggs
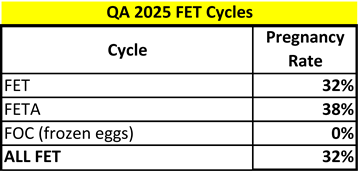
FROZEN-THAWED CYCLES WITH UNTESTED EMBRYOS -- Which brings us to frozen-thawed cycles (see below): Once again, considering the CHR’s patient population in which “excessive embryos” are a rarity, even if available, usually come from older women with many prior cycle failures. These numbers, therefore, are rather surprisingly high. The 0% rate for FOC was again consequence of almost no cases.
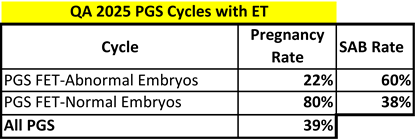
FROZEN-THAWED CYCLES WITH PGT-A TESTED EMBRYOS – Here it is important to point out that – since the CHR, with few exceptions, does not recommend PGT-A to its patients– here listed cycles mostly involve patients who moved their – elsewhere produced “euploid” and “aneuploid” embryos (the “ – “ is reflective of the CHR’s skepticism about PGT-A results) - to the CHR. These cycles, therefore, are reflective of the only here reported patient population not representative of the adverse prognostic selection of all other here reported patients and is more reflective in age and other characteristics of a typical U.S. IVF clinic patient population.
What we here want to comment on is the fact that the 80% clinical pregnancy rate in “euploid” PGT-A tested embryos is, likely, an artefact due to very small cycle numbers (patients, of course, only rarely have reasons to transfer “normal” PGT-A tested embryos to the CHR, while they have very good reasons to transfer “aneuploid” embryos since most IVF clinics, still, reject transfers of all “aneuploid” embryos, - even “mosaic” embryos.)
The here reported clinical pregnancy rate from transfers of “aneuploid” embryos is, however, again worthwhile to point out and was, indeed, similar to the rates we previously reported in several publications from the CHR’s registry of such cycles. This, - despite the fact that we are now starting to encounter an increasing number of patients with “aneuploid” embryos who insist on having embryos transferred which the CHR does not recommend for transfer. Patients in those cases, therefore, are transferred these embryos only after they sign “against medical advice” consents.
Summary and Conclusions
Though preliminary, here presented 2025 outcome data reaffirm the CHR’s IVF practice which serves primarily a patient population otherwise completely ignored by the IVF field and practically uniformly offered only third-party egg donation as a treatment choice.
And while pregnancy and live birth outcomes in such a patient population, of course, significantly lag behind national averages, - considering the adverse selection of the CHR’s patient based on (significantly older) age, number of prior failed IVF cycles, ovarian reserve parameters, and other confounders – these, by now very consistent data, not only must be considered exception but must also be considered evidence that current U.S. and worldwide IVF practice - which practically withholds autologous IVF from women above age 42 to 43 years - must be revisited.
This conclusion does not only apply to IVF clinics but also to insurance companies and even governments which often age-restrict access to IVF coverage at unreasonably young ages based on outdated outcome data which no longer have relevance.
This statement is, however, also based on the recognition that older ovaries must be treated differently form younger ovaries (whether they sit in younger or older bodies): The CHR – by now over a decade ago - for the first time discovered that follicle maturation speeds up with advancing age and that, therefore, oocytes must be retrieved at progressively smaller follicle sizes.1,2 We , in parallel, learned from publications in the literature that the exogenous gonadotropins currently available for fertility treatments become with advancing age increasingly toxic to ovaries (currently available gonadotropins in their glycosylation patterns unfortunately do not follow nature’s example).3
Becoming aware of these and other age-dependent changes in ovarian physiology, the CHR has been – and continuous to – adjust IVF cycles accordingly, - after all those years resulting in an IVF cycle in older women which is systemically different from traditional IVF cycles. And until other IVF clinics recognize that older ovaries must be treated radically differently from how ovaries have routinely been treated in IVF for over 40 years, their cycle outcomes will remain poor, - reinforcing the vicious cycle of believing that IVF in women over age 43 only produces pregnancy rates of 1% t0 2%.
REFERENCES
1. Wu et al., J Endocrinol 2015;226(3):167-180
2. Wu et al., J Ovarian Res 2018;11:23
3. Bernstein et al., Reprod Biol Endocronol 2024;22:52